Special Populations
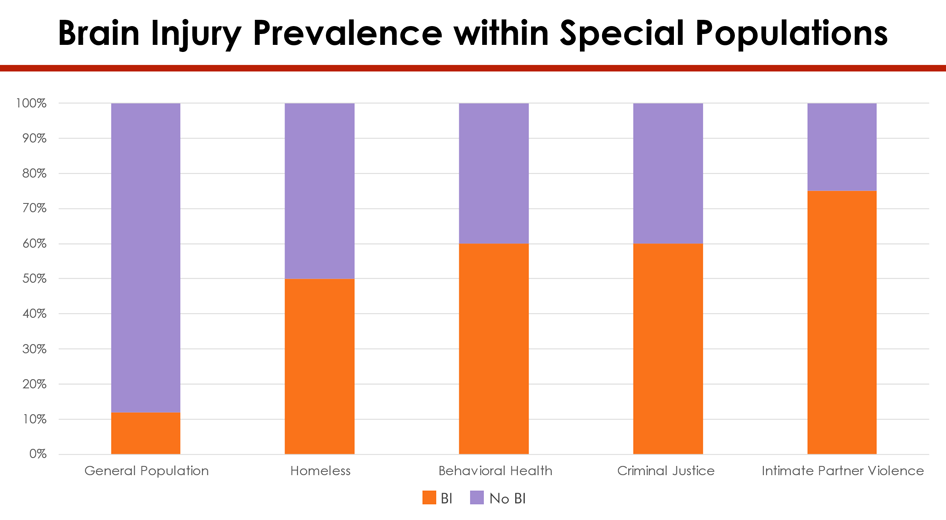
When we look at the research on what types of individuals sustain brain injuries, there are certain populations of people that are over represented. Twelve percent of the general population have a history of brain injury, while the homeless population prevalence is 50% with the majority of those injuries being sustained prior to homelessness. Behavioral health (mental health and substance use disorders) prevalence of brain injury is 60%. Those involved in the criminal justice system also have a prevalence rate of 60%, and those having experienced interpersonal violence have a rate of 75%.
The North Dakota Brain Injury Network (NDBIN) finds these numbers unacceptable and is making efforts to reduce the number of brain injuries among these special populations. Learn about resources and information specific to each of these special populations.
- Criminal Justice
- Homelessness
- Intimate Partner Violence
- Mental Health
- Substance Use
- Suicidality After Brain Injury
 Criminal Justice
Criminal Justice
The American criminal justice system has a large number of inmates with a history of brain injury. There are many contributing factors to this statistic, and we at NDBIN know that North Dakota can help reduce this number.
Ways NDBIN Can Help
- Support groups – We can advertise and refer individuals to groups and provide or help find facilitators.
- NDBIN can help support groups access Specialized Support Group Curriculum – These curriculums work on understanding the makeup of the brain, the injury, and the healing process through structured activities and information sharing.
- NDBIN, in partnership with the North Dakota Department of Corrections, has begun screening residents of the North Dakota State Penitentiary and offering Living Life Fully training to help residents learn about and live with a brain injury.
- Read about NDBIN's work with incarcerated brain injury survivors in this article, Paving a Path to Resilience.
- Resource facilitation – Call or email NDBIN, and we can help you find resources in your area that are appropriate for you.
- Peer-to-Peer Mentoring involves pairing individuals with peer support specialist.
Resources
 Homelessness
Homelessness
Often brain injury and homelessness work in tandem. Ninety percent of individuals with a brain injury report that their first injury was sustained prior to becoming homeless.
Individuals with a history of traumatic brain injury who also experience homelessness tend to struggle with:
- Physical and mental health
- Substance use
- Suicidal ideation or attempts
- Memory
- Involvement in the criminal justice system
Resource
 Intimate Partner Violence
Intimate Partner Violence
Unfortunately, many individuals, women in particular, are overrepresented in the brain injury world due to interpersonal violence. If someone is hurting you, please get help! For more information on resources to help get you out of these unhealthy relationships, call (855) 866-1884 or email info@ndbin.org.
Resources
- Brain Injury and Intimate Partner Violence Infographic
- Invisible Injuries Packet
- Invisible Injuries Rack Card
 Mental Health
Mental Health
Oftentimes, individuals with a brain injury struggle with mental health issues, such as anxiety and depression. There are many options for you to try to get a handle on these issues.
Resources
- North Dakota Mental Health Providers
- Emotional Dysregulation
- Brain Injury & Mental Health Infographic
 Substance Use
Substance Use
Substance use following brain injury can be a slippery slope. After individuals sustain injuries, their inhibitions become lowered, allowing them to be much more susceptible to using and, under certain circumstances, misusing substances.
Resources
- Traumatic Brain Injury and Substance Use Disorders: Making the Connections – The National Association of State Head Injury Administrators (NASHIA) partnered with the Mid-America and Mountain Plains Additions Technology Transfer Centers and Dr. Carolyn Lemsky to produce a toolkit for addictions.
- Client Workbook: Substance Use and Brain Injury – NASHIA produced this workbook, written by Dr. Carolyn Lemsky and Dr. Tim Godden, as a resource for people who are living with the effects of a brain injury and are wondering how their substance use may be affecting them.
- Substance Abuse as a Mediating Factor in Outcome from Traumatic Brain Injury – If you heard anyone from NDBIN present before, you've probably heard us reference John Corrigan's study on brain injury and alcohol.
- Substance Use and TBI – This FREE online course offered by NDBIN covers the impact a brain injury can have on substance use disorder and treatment approaches for working with individuals with brain injury.
- Brain Injury & Substance Abuse Infographic
 Suicidality After Brain Injury
Suicidality After Brain Injury
Research has shown that people with brain injuries have a significantly higher risk of suicidal thoughts, attempts, and death by suicide compared to the general population.
All types of brain injury can lead to these symptoms:
- Neurological changes – Damage to areas like the frontal lobe (which controls impulse regulation, emotional processing, and decision-making) can lead to poor emotional control and impulsive behavior.
- Cognitive and emotional effects – Brain injuries often cause depression, anxiety, irritability, and hopelessness—key risk factors for suicide.
- Chronic pain or disability – Ongoing pain, fatigue, or loss of independence can lead to despair or isolation.
- Social and vocational losses – Many people with brain injuries lose jobs, relationships, or social roles, which can heighten feelings of purposelessness.
- Substance use – Some survivors turn to alcohol or drugs to cope, which can worsen depression and impulsivity.
Brain injury affects mental health. After a concussion or traumatic brain injury (TBI), the brain may have difficulty regulating:
- Emotions (feeling overwhelmed, hopeless, or unusually sad)
- Impulses (reacting quickly without thinking through consequences)
- Stress (reduced ability to cope with everyday pressures)
- Sleep (insomnia or disrupted sleep can worsen mood)
- Thinking clarity (brain fog can create frustration or anxiety)
These changes can make someone more vulnerable to depression, anxiety, and suicidal thinking, sometimes months or years after the injury.
Facts and Statistics
- People with concussion or mild TBI had approximately twice the risk of death by suicide compared to uninjured controls.
- People with TBI also show elevated rates of suicidal thoughts (ideation) and suicide attempts.
- A large meta-analysis reported that about 19% of individuals with TBI experience suicidal ideation and about 2% have attempted suicide.
- Suicidal ideation has been reported consistently across follow-up years, and individuals with early post-injury suicidal behavior remain at higher risk long term.
- Clinical guidelines recommend routine screening for suicide risk and mental health symptoms among people with TBI, especially in the first years post-injury when risk is highest.
Further Assistance
If you or someone you know is struggling:
- Call or text 988 to reach the Suicide and Crisis Lifeline, available 24/7.
- NDBIN supports survivors of brain injury with symptom management. Contact us to get set up with a resource facilitator.
- View references.